Varicose Veins
What Are Varicose Veins?
Varicose veins are normal veins (blood vessels) that become abnormally dilated or widened due to venous pressure.
Affected veins typically become visible and appear swollen, twisted. Varicose veins protrude or bulge above the skin’s surface. Varicose veins appear as blue, purple, or red veins.
Varicose veins may also be known as Venous Insufficiency Syndrome and is often the result of a deeper, underlying venous disease.
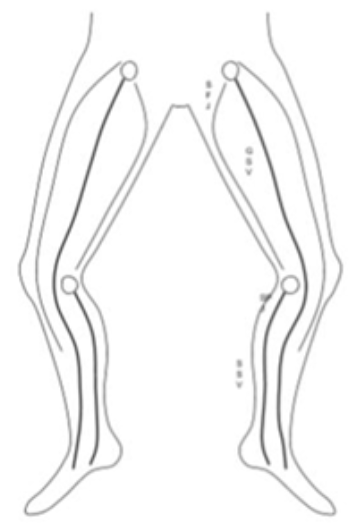
Where Do Varicose Veins Occur?
Varicose Veins are most common in the superficial veins of the legs. Varicose veins are easily found and typically appear first on the:
- Back of the calf
- On the inside of the leg
- Upper thighs
However, Varicose Veins can form elsewhere in the body.
What Do Varicose Veins Look Like?
These differ from spider veins, as they are larger, however they similarly twist and turn. These visible varices may vary depending on the stage or severity of the condition.
Who Is at Risk of Varicose Veins?
Varicose veins risk factors can often be related to stress brought on the legs.
While generally, anyone can be at risk of varicose veins, the condition is more likely in people who are:
- Likely to have defective valves
- Prone to blood clots
- Women
- Genetically-prone (i.e. the condition runs in the family)
- Overweight
- Older
- Inactive or lack exercise
- Pregnant
Who Does Varicose Veins Affect?
About 14% of the adult population suffer from Varicose Veins, versus 59% for Spider Veins. More often found in older patients.
Varicose Veins on Women
Women are more likely to get varicose veins than men.
Females are more at risk due to other vein-strains including hormonal changes, puberty and pregnancy.
Varicose Veins on the Aged or Older People
While varicose vein onset typically occurs with age, often varicose veins can occur in patients aged in their mid-twenties.
While the actual bracket on age isn’t absolute, one may start seeing signs of varicose veins as early as their late twenties or early thirties.
Varicose Veins on Lighter Skin Types
This condition is more likely with lighter skin types.
Causes of Varicose Veins
Leg muscles pump the veins to return blood to the heart (the skeletal-muscle pump), against the effects of gravity.
Veins have pairs of leaflet valves to prevent blood from flowing backwards (retrograde flow or venous reflux).
When veins become varicose, the leaflets of the valves no longer meet properly, and the valves do not work (valvular incompetence). This allows blood to flow backwards and they enlarge even more.
Varicose Veins occur when the valves in the veins do not function properly and the blood leaks down and collects in the veins. This causes the veins to enlarge.
- Pregnancy
- Blood clots and other circulatory problems
- Hormonal changes including Puberty, Birth Control Pills
- Predisposition due to genetics
- Inflammation of the veins
- Injury or local trauma
- Sitting or standing for a long time
- Excess weight
Unknown Causes of Varicose Veins
While varicose vein causes are numerous and well-understood, diagnosing causes that aren’t listed above can often be attributed to certain lifestyles.
People prone to varicose veins can include lifestyle causes such as inactive lifestyles, obesity, people who have jobs that require them to stand for long periods of time.
Do Abnormal Veins Improve Over Time?
Abnormal leg veins (varicose veins or Varicose Veins) do NOT improve over time.
Varicose Veins left untreated do progressively worsen over time and at an accelerating rate – this means that Varicose Veins left untreated cause more Varicose Veins to appear over time, than if the Varicose treated in the first instance.
The well-understood problem of tooth decay and the risk of loss of a viable tooth if left untreated, serves as a good comparison.
How Do Varicose Veins Affect You?
Varicose veins is typically a superficial condition but can be a cosmetically disfiguring condition. Rarely are they regarded as a serious condition?
Besides unsightly web-like veins being visible, varicose veins do not pose any threat to one’s health. More advanced cases of varicose veins might cause heavy limbs or cramping pain especially when standing.
Varicose veins may spread to different parts of the body or when its causes are associated with more serious underlying conditions. If left untreated can lead to more serious health outcomes.
Why Do Varicose Veins Form?
Your blood is carried through veins to all parts of your body. While the heart pumps the blood, the veins use valves to stop the blood flow from moving backwards especially when gravity is pulling in another direction as occurs in your legs.
If the veins valves become weakened, blood can leak backwards into the veins and collect there.
This problem is called venous insufficiency. When backed-up blood makes the veins bigger, they can become twisted, lengthened, and swollen (another adjective for this is varicose).
What Are the Signs of Varicose Veins?
Over 75% of people with varicose veins have symptoms that interfere with their lives. People may experience visible indications in their legs including:
- Discoloured skin particularly around the ankle veins
- Twisted or bulging veins that are seen just underneath the surface of one’s skin
- Scaly or Dry skin
- Swelling or Heaviness
- Skin Ulcers
Varicose Veins Symptoms
Beyond the visible signs of varicose veins, other symptoms of varicose veins can experience feeling or sensations in the legs including:
- Tingling or numbness in the leg
- Burning sensations in the leg
- Restless type sensations in the leg
- Throbbing or cramping of legs
- Leg pain, muscle fatigue, tired and achy
- Leg cramping
- Bleeding in affected areas
- Irritation or Itchiness on the ankle or lower leg
What Related Disorders Occur with Varicose Veins?
The widening of a patient's veins that can cause Varicose Veins can also be related to increased venous pressure.
Other conditions or pathology can be associated with Varicose Veins. While rare, some complications are life-threatening.
Associated Conditions With Varicose Veins Include:
- Spider veins
- Deep Vein Thrombosis
- Lymphedema
- Dermatitis
- Thrombophlebitis
- Telangiectasias
- Varicoceles
- Pigmentation
- Hypotension
- Fainting Episodes
Severe Long-Standing Varicose Veins Can Lead To:
- skin thickening (lipodermatosclerosis)
- ulceration
- leg swelling
- venous eczema
What Is the Difference Between Varicose Veins and Venous Insufficiency?
Both Varicose Veins and Venous Insufficiency are chronic venous disorders which can include all structural and functional abnormalities of the venous system.
Venous insufficiency is more about the functional abnormalities of a patient’s veins and Varicose Veins can be a result of this condition.
Venous Insufficiency can produce advanced symptoms like oedema, skin changes or leg ulcers.
What Is Evident with Varicose Veins?
Varicose Veins could be an early warning of more serious underlying conditions that need to be treated, either through a doctor or through self-treatment.
Either way, the diagnosis should be made by our doctor before one proceeds by any means.
Varicose veins may also be known as venous insufficiency syndrome. This is a fairly common condition, with studies showing as many as 10% of men and 30% of women commonly consulting for venous symptoms and signs.
Stages of Varicose Veins
Stage 1 - Spider Veins
Early stages of varicose veins are purely seen on the skin. These dilated veins and capillary vessels are called telangiectasias.
Stage 2 - Pre Varicose Vein Stages
During the Pre Varicose Veins Stage, patients can observe a few signs, but patients start to become aware of early vein diseases.
The best time to have veins treated is when symptoms begin to develop. Left untreated, it can lead to more serious issues and vein diseases and even irreversible damage of the lymphatic system.
Stage 3 - Advanced Varicose Veins And Swelling
As the vein disease progresses, swelling of the legs may begin to occur but typically does not include Skin Changes.
The backflow in the venous system interferes with the body’s ability to reabsorb fluid leading to swelling of the leg.
Leg swelling caused by the retention of fluid in leg tissues is known as peripheral edema. It can be caused by a problem with the circulatory system, the lymphatic system or the kidneys. Swelling due to fluid buildup after sitting or standing for a long time may also occur.
Elevation may help with the symptoms, but will not cure venous disease. While swelling in the leg is commonly associated with vein diseases, there may be other underlying causes for swelling of the legs.
This stage can include the growth of the varicose veins to larger areas of the skin. It also includes pain, more swelling as well as muscle aches on the affected areas.
Stage 4 - Skin Discolouration Without Ulcers
As the vein disease progresses, venous congestion may lead to changes in the skin’s color. The skin may also become thinner and discoloured to reddish-brown or whitish in color. At this stage, the skin is easily injured and takes more time to heal.
During this stage, skin irritation and bleeding become more common.
Stage 5 - Skin Discolouration With Ulcers
The skin colourisation can spread beyond local varicose veins and lead to ulceration particularly around the ankles.
Stage 6 - Advanced Skin Ulceration
Venous ulcers usually occur due to improper functioning of a patient's veins and valves. This stage is the most advanced form of Superficial Vein Diseases.
Venous ulcers also are known as venous insufficiency ulceration, stasis ulcers, stasis dermatitis, varicose ulcers, or ulcus cruris are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs (hence leg ulcers).
Leg and ankle ulcers are caused by venous congestion that has progressed, to a point where it can have serious consequences.
It means a patient's blood flow is insufficient to provide nutrition to the skin. Once vein diseases have progressed to this stage, any type of skin injury will only heal slowly.
Without treatment, skin ulcers can remain unhealed for an extended period of time, and more than likely get worse.
These venous ulcers can become chronic wounds if left untreated and can be extremely painful. Cellulitis or leg infection may occur, increasing the risk of sepsis or blood infection.
Why Treat Varicose Veins?
Many who opt for varicose vein treatment are unhappy with the unsightly marks that appear on the surface of their skin, so they may observe a boost of confidence when the condition is treated. This is especially true for more severe cases of the condition where it has spread to varying areas of the skin.
When Should I Consider Watchful Waiting of Varicose Veins?
Watchful waiting of varicose veins should never be considered. Varicose Veins will never improve spontaneously. Existing varicose veins cause new varicose veins to appear at an accelerated rate.
Types of Varicose Vein Treatment
Varicose vein emergence is unsightly and may lower one’s self-esteem. This is especially true for advanced stages of the condition.
Varicose veins can be treated by either clinical treatment or lifestyle changes. The latter affects the condition much slower than the former, so that may be a consideration that affects one’s course of action.
Treatment choices for Varicose Veins incude:
- Sclerotherapy
- Laser Therapy
- Phlebectomy
Alternative Treatments for Varicose Veins
Additional or Alternative treatments or non-surgical treatments for Varicose Veins include Elastic Compression Socks or Compression stockings.
Varicose Veins Prevention
There is no known method of prevention.
Wearing specialised venous support stockings may prevent some dilated blood vessels from developing in some people.
Maintaining a normal weight and regular exercise, especially walking, may also be helpful.
Certain footwear may restrict normal ankle movement and these include high heeled shoes. So people who are susceptible to venous disease should avoid wearing this type of footwear.
Lifestyle Recommendations for Preventing Varicose Veins
To prevent varicose veins, patients are advised to improve circulation in the veins. For some, this may require lifestyle changes:
- Avoid sun exposure, especially if of a lighter skin type
- Reduce weight as obesity will increase the risk of pressure being exerted on the blood walls
- Avoid wearing tight clothes which may interrupt the circulation
- Avoid wearing high heeled shoes as calf muscles put in a lot of energy when you try to walk in heels, when the calf muscles are at rest the circulation will be improved
- Circulation can be improved by following the convention methods listed
- Exercise and Physical activity should be included in your daily routine
- Avoid sitting for long hours without standing up for a break
- Avoid standing for hours without significant movement
- Avoid putting pressure on veins by resting them periodically
Recurrence of Varicose Veins After Treatment
Ongoing checking for any re-emergence of varicose veins is recommended after completion of treatment for varicose veins .
The likelihood of Recurrence of Varicose Veins is high in patients with a genetic predisposition. Where the cause is of a genetic nature, more active prevention may also be required.
Varicose Veins are also likely to come back with age or if other causes are not addressed such as:
- Lack of physical exercise or an inactive lifestyle
- Standing for long periods of time
- Undertaking ineffective treatments
It is best to consult a doctor and seek treatment, especially when recurrence causes any sort of pain or discomfort.
Preventing Varicose Vein Recurrence
Further treatment can be avoided by living a healthier lifestyle and applying preventive measures that are similarly used to treat the condition.
Lifestyle Recommendations for Preventing Varicose Veins from returning include:
- Resting them periodically
- Avoiding wearing high heels
- Maintaining a healthy weight as to avoid putting extra stress on your circulation
- Avoiding standing for hours without significant movement
Periodic Vein Screening
Consult the appropriate doctor to screen for any other vein complications you may be at risk for. An appropriate assessment that gauges how likely you are to suffer from venous diseases is even more urgent if you have recurring vein disease.